Title: Rapid, label-free CD4 testing using a smartphone compatible device
Authors: Manoj Kumar Kanakasabapathy, Hardik J. Pandya, Mohamed Shehata Draz, Manjyot Kaur Chug, Magesh Sadasivam, Shreya Kumar, Behzad Etemad, Vinish Yogesh, Mohammadali Safavieh, Waseem Asghar, Jonathan Z. Li, Athe M. Tsibris, Daniel R. Kuritzkes, and Hadi Shafiee
Year: 2017
Journal: Lab on a Chip
http://pubs.rsc.org/en/content/articlelanding/2017/lc/c7lc00273d
There have been many fantastic advancements in the treatment of HIV/AIDS in the past few decades, including developing reliable testing methods and ways of treating the disease (like antiretroviral drugs that work against the virus in the body). However, effectively treating HIV depends on quickly diagnosing and determining the severity of the disease. While this process is usually fast in the richer areas of the world, it can be harder in poorer areas. If the diagnostic equipment and medicine are hundreds of miles away, it could take weeks or even months to know if a person has HIV, wasting time when they could be receiving treatment.
In this article, the authors developed and tested a new HIV detection device that is small, cheap, and easy to use; all it needs is a drop of blood and a smartphone. The device is based on determining the concentration of CD4+ T-cells in the blood. These are immune cells that HIV infects and kills. Because of this, people with HIV have a reduced number of CD4+ T-cells, called a “CD4 count.” Healthy people typically have 500 to 1600 cells per microliter (cells/µL), but people with suppressed immune systems (like those with HIV) have counts below 500.
The device itself is made from a glass slide glued to an acrylic sheet. The acrylic is cut so there is a channel underneath its surface that runs along the glass. This works like a pipe that liquid can flow through and make contact with the surface of the glass. The glass is then silanized, where long alkoxysilane molecules are chemically bound to the surface of the glass (Figure 1.i). In this experiment, silane-polyethylene glycol-thiol (silane-PEG-SH) was used. The thiol group at the end of the molecule is used as the acceptor to an additional linker molecule, 3-(2-pyridyldithio)propionyl hydrazide (PDPH) (Figure 1.ii). Finally, this reacts with an oxidized antibody, anti-human CD4, which is a protein that binds to CD4+ T-cells (Figure 1.iii-iv). To make sure these molecules were actually attached, the authors used Fourier-transform Infrared spectroscopy (FTIR) (an instrument that determines the bonds and functional groups in a material).

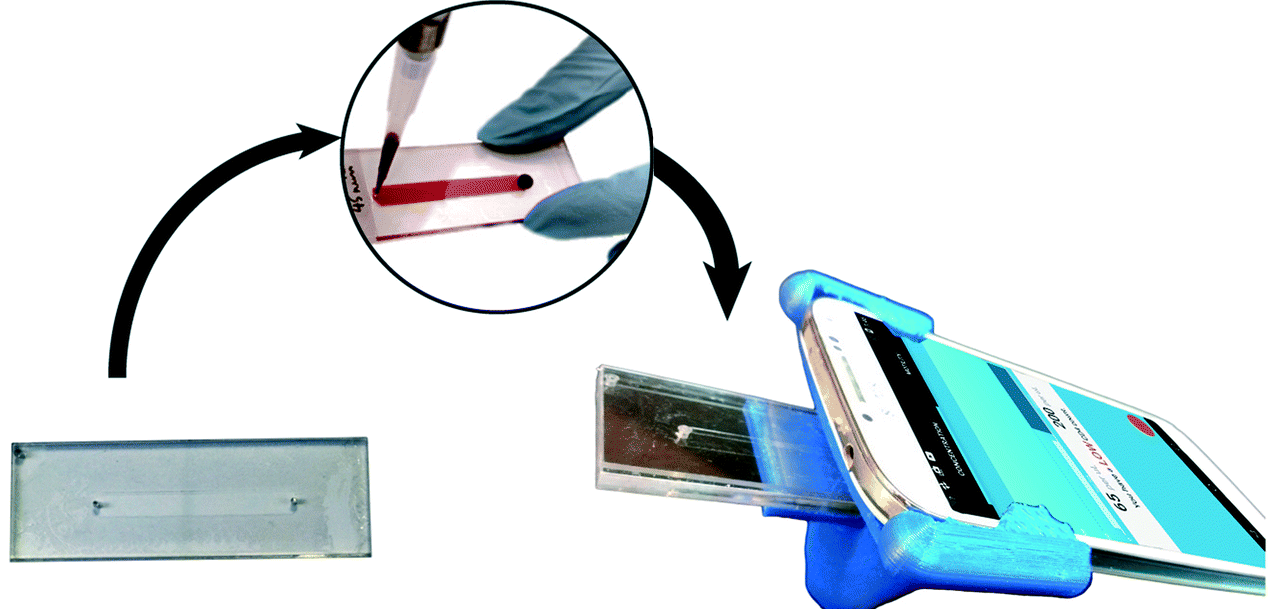
Because the anti-human CD4 antibody is chemically attached to the surface of the glass slide, any CD4 T-cell that it binds to will be attached as well. This is the basis of the detection method. Blood is added into the device so it makes contact with the antibodies on the glass slide and allowed to sit for 30 minutes to make sure that all CD4+ T-cells are bound to the antibodies. Then, all remaining cells are washed away and the slide is placed in a custom-made holder. This device contains a small, battery-powered light and two lenses, taken from a DVD and CD drive. When the device is placed on a smartphone, these lenses turn the phone’s camera into a miniature microscope (Figure 2A). Because the dimensions of the area the camera can see are known, custom software is able to count the number of visible CD4+ T-cells and calculate a concentration in terms of cells/µL.
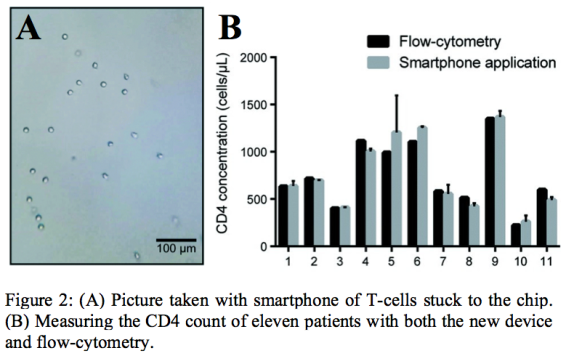
The authors tested their device using several solutions with specific concentrations of CD4+ T-cells ranging from 60 cells/µL to 1200 cells/µL. They compared the CD4 count from their device with one measured using a flow cytometer, the most widely used detection method. Looking at the data, the smartphone device’s results were extremely similar to the flow cytometer. Also, the authors tested the whole blood (unprocessed and unfiltered blood) of eleven people, some of whom were HIV-positive. The CD4 counts determined by the authors’ device and the count from flow cytometry were found to have no statistically significant difference, showing that the device was accurate when used with real-world blood samples (Figure 2B).
The benefit of using such a device over expensive, non-traveling instruments (like a flow cytometer) could eventually save lives. The authors estimate that each chip used in the device costs less than $2 to make, while the portion containing the lenses that attaches to a smartphone costs less than $2.75. This means that for around $100, fifty people could be tested for HIV. Also, because the device can give a CD4 count within an hour of taking the blood sample, patients are much more likely to get treatment as soon as possible, which is one of the most important factors in treating HIV. Fast, cheap, and portable medical screening devices like this one have the potential to help huge numbers of people all around the world.